by Author Howard Markel, MD, PhD – ICPA.org:
Attention Deficit Disorder and Ritalin
The boy is 14 years old and has one of the most severe cases of attention deficit disorder (ADD) that I have seen as a pediatrician. He fidgets; there are nonstop hand gestures, leg swinging and tapping. More troubling, he simply will not pay attention to any adult attempting to engage him in conversation, placing him in great jeopardy of flunking out of school.
During his first office visit, the boy explained his predicament to me: “It’s like I’m in a room with 20 big screen HDTVs blaring away in surround-sound. And on them are all the newest videos from MTV. The problem is that I can’t decide which one to watch, so I try to watch them all.”
His mother is less focused on her son’s perpetual motion than on his angry outbursts and what she sees as his refusal to listen to her. The day we met, she had already decided what she wanted to do. I was being told to write a prescription for Ritalin.
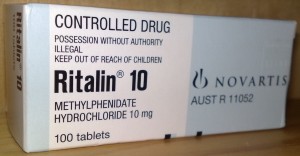
As every pediatrician knows, stimulant drugs like methylphenidate (Ritalin) cause most people to speed up their actions and thoughts. But for those with ADD (with or without hyperactivity), these drugs can slow them down, reduce overactivity, increase attention span, and can even improve relationships between a child and parents or other family members. There are, however, some nagging problems: none of us is exactly certain how these drugs work or what their long-term benefits and risks might be. Sometimes, they cause intolerable side effects such as tics and sleep disturbances.
The young man was clearly unhappy with his mother’s decision and let it be known with a slew of scowls and outcries of “Shut up!!” I asked him why he would prefer not being able to pay attention to his schoolwork, to which he replied: “You just don’t get it. I’m a lot more fun when I don’t take Ritalin. I crack great jokes in class and my friends think I am really cool. But when I take that stuff, I’m zoned out. I’m like a log. Ritalin ruins my life.”
This description went a long way in explaining why many teachers (and not a few parents) of kids with ADD prefer their charges to be medicated and why many children resist such attempts. Left untreated, however, many of these kids create problems with disruptive behaviors and can destroy the normal dynamics of a classroom and at home.
Here was my dilemma: The boy’s mother, and not the young man, wanted the prescription. The law defines a 14-year-old as a minor, but given that his condition was hardly fatal and essentially a behavioral issue, to whom should I have listened? The mother, who wants a more controllable child, or the boy, who simply wants to be what he perceives to be his true self? After all, the essence of adolescence is finding out who you are and figuring out who you want to be. As a pediatrician, I am supposed to be assisting youngsters in this difficult process.
That day, I listened to the parent and wrote the standard prescription for 40 mg of Ritalin a day. Like millions of youngsters with ADD, he takes 20 mg before going to school in the morning and another 20 mg at lunch.
Every month, I see the boy to renew his prescription for Ritalin and to make sure that there are no serious side effects. At each visit, he greets me with a deep-rooted but quiet anger. His fidgeting and outbursts seem to have diminished, but there has been little improvement in his schoolwork. Last year, he barely passed the eighth grade and his mother admitted that 2 of his teachers simply elected to pass him to avoid a repeat year with him. Nevertheless, she is delighted with the results.
When the boy is on vacation from school, I have noticed a definite change in his demeanor. Typically, when school is out, pediatricians give children with ADD a “drug holiday.” When he does not take his medication, his fidgeting and inattention are back in full force but he beams with joy, at least when I see him, and tells me that without Ritalin he can again enjoy cutting up in front of his friends.
But in his mother’s defense, I don’t live with him and have no real idea how disruptive his ADD behaviors can be at home. In cases like these, I have to listen to the parent that does live with him. I remain terribly conflicted about pharmacologically altering this young man against his will. Using potent pills to treat a disorder we do not completely understand flies in the face of prudent medical practice, and yet we pediatricians do this all the time with our ADD patients. More than a century ago, the great physician Sir William Osler observed that “the desire to take medicine is one feature which distinguishes man, the animal, from the rest of his fellow creatures.” In the practice of pediatrics, we are often compelled to include the parent’s desire in that rubric.
But still, I wonder, am I doing the right thing?
Article originally posted at ICPA.org.